Example Of Soap Note Nursing . Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. As you work on becoming. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. Find free downloadable examples you. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. It is the documentation used to record information about encounters with. Soap nursing notes are a type of patient progress note or nurse’s note. Soap note examples, templates and format guide.
from www.etsy.com
The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. As you work on becoming. It is the documentation used to record information about encounters with. Find free downloadable examples you. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. Soap nursing notes are a type of patient progress note or nurse’s note. Soap note examples, templates and format guide.
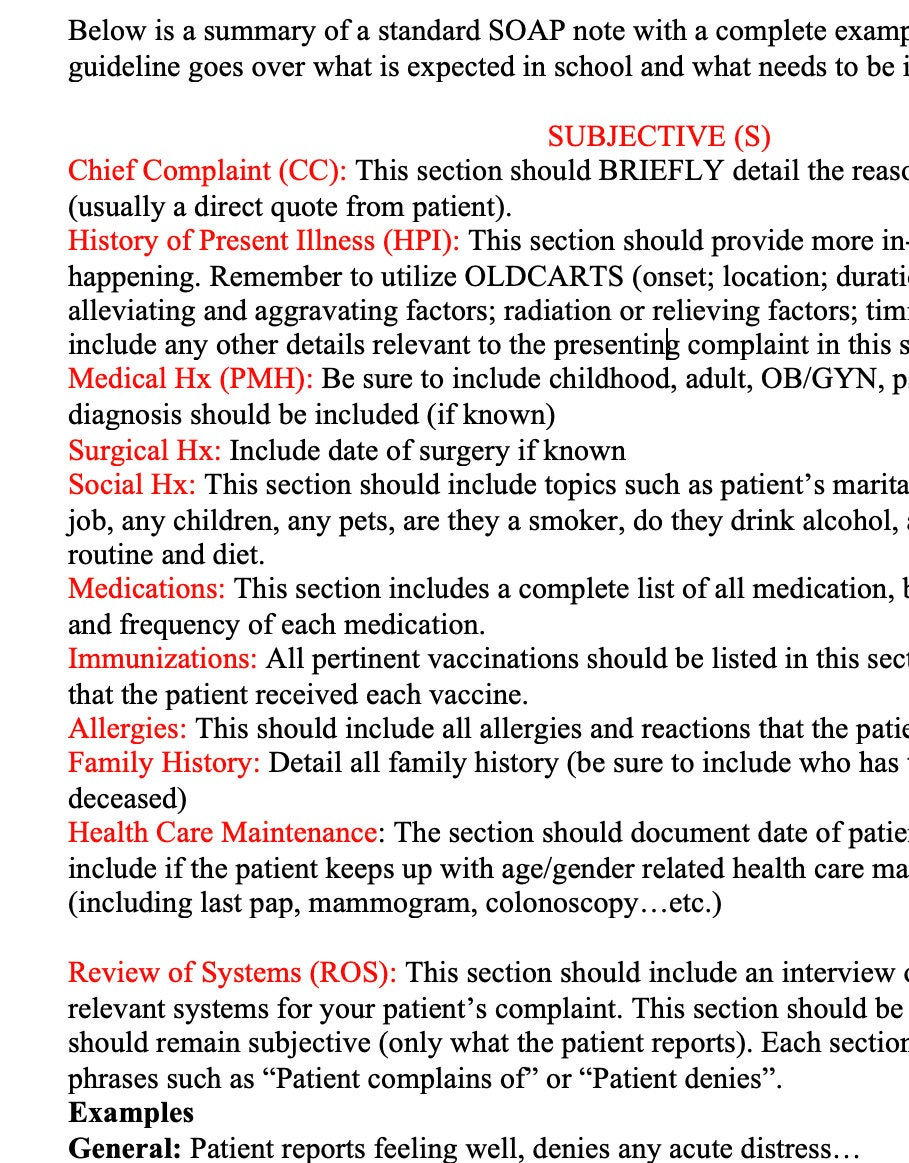
SOAP Note Guide and Real Example for Nurse Practitioners, Physician Assistants, Providers, and
Example Of Soap Note Nursing Soap nursing notes are a type of patient progress note or nurse’s note. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Find free downloadable examples you. It is the documentation used to record information about encounters with. Soap nursing notes are a type of patient progress note or nurse’s note. As you work on becoming. Soap note examples, templates and format guide. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Example Of Soap Note Nursing Soap nursing notes are a type of patient progress note or nurse’s note. Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. As you work on becoming. It is the documentation used to record information about encounters with. Soap notes are a widely used and accepted format by healthcare practitioners, from mental. Example Of Soap Note Nursing.
From idtcenter.org
Free Free 19 Soap Note Examples In Pdf Examples Nursing Soap Note Template Excel IDTcenter Example Of Soap Note Nursing As you work on becoming. It is the documentation used to record information about encounters with. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Soap. Example Of Soap Note Nursing.
From www.calypsotree.com
10 Amazing Soap Note Examples Calypso Tree Example Of Soap Note Nursing Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Soap note examples, templates and format guide. Soap nursing notes are a type of patient progress note or nurse’s note. As you work on becoming. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians. Example Of Soap Note Nursing.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Example Of Soap Note Nursing It is the documentation used to record information about encounters with. Find free downloadable examples you. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Soap nursing notes are a type of patient progress note or nurse’s note. The subjective, objective, assessment and plan (soap) note is. Example Of Soap Note Nursing.
From www.highfile.com
Nursing SOAP Note Template Word PDF Google Docs Highfile Example Of Soap Note Nursing Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Soap note examples, templates and format guide. As you work on becoming. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. Find free downloadable examples you. It is the documentation used to. Example Of Soap Note Nursing.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab Example Of Soap Note Nursing An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. It is the documentation used to record information about encounters with. Soap note examples, templates and format guide. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social.. Example Of Soap Note Nursing.
From www.pinterest.fr
soap note examples for nurse practitioners Nursing Documentation Examples, Nursing Notes Example Of Soap Note Nursing It is the documentation used to record information about encounters with. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. Find free downloadable examples you. As you work on becoming. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and. Example Of Soap Note Nursing.
From www.etsy.com
SOAP Note Guide and Real Example for Nurse Practitioners, Physician Assistants, Providers, and Example Of Soap Note Nursing As you work on becoming. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Soap nursing notes are a type of patient progress note or nurse’s note. It is the. Example Of Soap Note Nursing.
From mungfali.com
Sample Nursing Soap Note Example Of Soap Note Nursing The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. As you work on becoming. Find free downloadable examples you. It is the documentation used to record information about encounters with. Soap nursing notes are a type of patient progress note or nurse’s note. Learn how to write a. Example Of Soap Note Nursing.
From www.sampletemplates.com
FREE 15+ SOAP Note Templates in PDF MS Word Example Of Soap Note Nursing Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Find free downloadable examples you. As you work on becoming. It is the documentation used to record information. Example Of Soap Note Nursing.
From www.pinterest.com
Prescription Pad, Nursing Notes, Nursing Tips, Soap Note, Software Offers, Beginning Writing Example Of Soap Note Nursing Soap nursing notes are a type of patient progress note or nurse’s note. As you work on becoming. It is the documentation used to record information about encounters with. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. Soap note examples, templates and format guide. Find free downloadable examples. Example Of Soap Note Nursing.
From doctemplates.us
Nursing Cheat Sheet Template DocTemplates Example Of Soap Note Nursing As you work on becoming. Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method. Example Of Soap Note Nursing.
From www.highfile.com
Nursing Soap Note Example Word PDF Google Docs Highfile Example Of Soap Note Nursing An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Find free downloadable examples you. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap nursing notes are a type of patient progress note or nurse’s. Example Of Soap Note Nursing.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Example Of Soap Note Nursing Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. As you work on becoming. Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Find free downloadable examples you. Soap note examples, templates and format guide. It is the documentation used to. Example Of Soap Note Nursing.
From mungfali.com
Sample Soap Note Template Example Of Soap Note Nursing The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. It is the documentation used to record information about encounters with. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Soap nursing notes are a type. Example Of Soap Note Nursing.
From omnichannelretailingforum.com
soap note example nurse practitioner All You Need To Know Example Of Soap Note Nursing An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. It is the documentation used to record information about encounters with. Find free downloadable examples you. Soap nursing notes are a type of patient progress note or nurse’s note. The subjective, objective, assessment and plan (soap) note is. Example Of Soap Note Nursing.
From www.pinterest.com
SOAP Notes Dentistry Example Soap note, Nursing documentation, Nursing notes Example Of Soap Note Nursing As you work on becoming. Soap note examples, templates and format guide. Find free downloadable examples you. Soap notes are a widely used and accepted format by healthcare practitioners, from mental health professionals to physicians and social. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. Soap. Example Of Soap Note Nursing.
From www.pinterest.com.au
3+ SOAP Note Example Free Download Soap note, Nursing notes examples, Nursing notes Example Of Soap Note Nursing It is the documentation used to record information about encounters with. Learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. An effective soap note is a useful reference point in a patient's health record, helping improve patient satisfaction and quality of care. As you work on becoming. Find free downloadable examples you.. Example Of Soap Note Nursing.